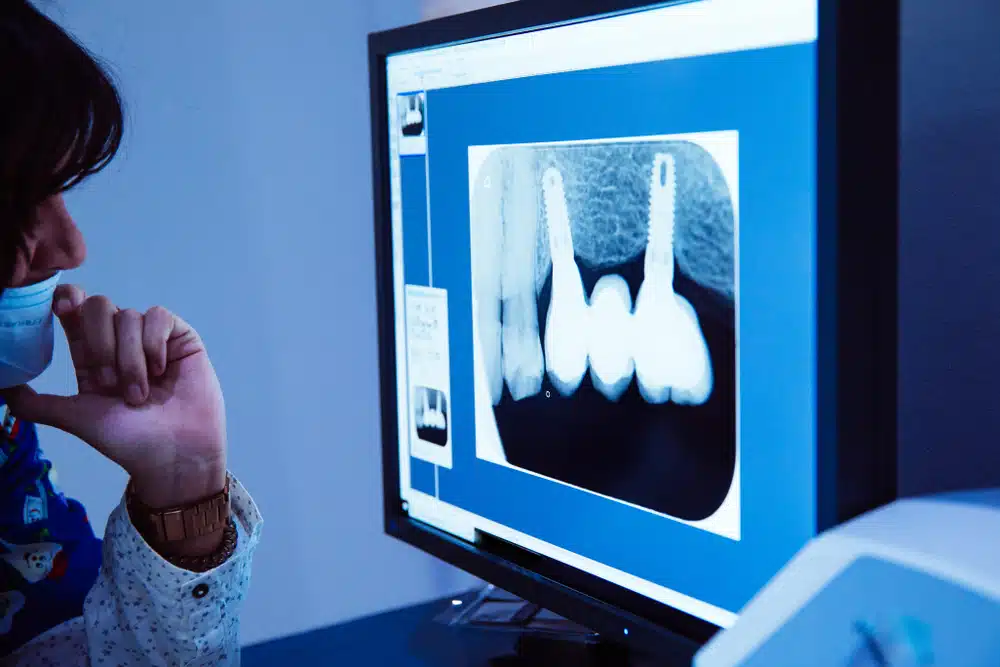
The Vital Role of Bone Preservation in Dental Health
Bone health is a crucial aspect of overall dental care, but its importance goes beyond just supporting our teeth. Both natural teeth and dental implants play significant roles in maintaining jawbone integrity. This blog explores how teeth and implants contribute to bone preservation, discusses the importance of ridge preservation when considering implants, and delves into the procedures and timelines involved in dental implantation.
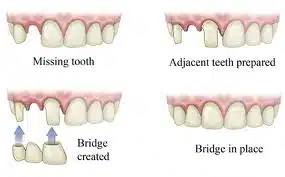
How Teeth and Implants Preserve Bone
Teeth: Natural teeth are embedded in the jawbone, and each time you chew, they stimulate the bone around them. This mechanical stimulation is critical for maintaining bone density and volume, as it signals the body to continually rebuild and repair the surrounding bone.
Implants: Like natural teeth, dental implants help preserve and stimulate the jawbone. When an implant is placed in the jaw, it acts similarly to a natural tooth root, providing the necessary stimulation to keep the bone intact and healthy. Without this stimulation, the bone area would resorb or shrink over time.
The Importance of Ridge Preservation
When teeth are extracted, it’s vital to consider ridge preservation to maintain bone health and volume. Ridge preservation involves placing a bone graft material into the tooth socket immediately after extraction. This procedure helps prevent the jawbone from collapsing and losing density, which is crucial for future implant placement or even for the aesthetics and functionality of dentures.
Materials Used in Ridge Preservation:
- Autografts: Bone taken from another site in the patient’s own body.
- Allografts: Processed bone obtained from a human donor.
- Xenografts: Bone derived from animal sources, typically bovine.
- Alloplasts: Synthetic bone-like materials.
These materials help support the structure of the jaw and provide a scaffold for new bone growth.
Bone Maturation Process
Bone maturation is a time-consuming process, typically taking several months. The timeline can vary depending on the individual’s health, the location of the graft, and the type of graft material used. Bone in the maxilla (upper jaw) generally takes longer to mature than in the mandible (lower jaw) due to differences in bone density and blood supply.
When to Consider a Sinus Lift
A sinus lift, or sinus augmentation, is necessary when there is insufficient bone height in the upper jaw, or the sinuses are too close to the jaw for implants to be placed. This procedure involves lifting the sinus membrane and placing a bone graft onto the sinus floor, allowing implants to be secured properly.
Guided Tissue Regeneration (GTR)
Guided tissue regeneration is a technique used to encourage the body to grow bone and tissue at an implant site. It involves placing a barrier membrane around the bone graft to protect it from fast-growing soft tissue, ensuring that bone cells have the space and time to proliferate. This technique is essential for successful implant integration.
Timeline and Phases of Dental Implant Procedures
The process of getting a dental implant can take several months to over a year, depending on the healing and bone maturation stages. The extended timeframe ensures that the implant is fully integrated into the bone, providing a stable foundation for the artificial tooth.
Immediate vs. Delayed Implant Placement
Some dentists prefer to place an implant immediately after tooth extraction to reduce the overall treatment time and preserve the bone. Others opt to wait until after a bone graft has matured to ensure the area is sufficiently stable to support the implant. The choice often depends on the specific conditions of the patient’s jawbone and overall dental health.
Using Sites with Existing Teeth for Implants
In cases where the jawbone is overly resorbed, sites that still contain teeth might be considered for implants. These areas can provide better bone quality necessary for successful implantation, especially if other regions are not viable due to severe bone loss.
___________________________
Understanding the complex interplay between bone health and dental treatments is key to maintaining a healthy, functional smile. Whether through natural teeth or implants, preserving jawbone integrity is essential. For anyone considering dental implants, being informed about the procedures, materials, and timelines involved can make the journey smoother and more predictable.