by Dr. Richard J. Walicki | Oct 23, 2025 | Dentistry, Leaky gut
If you’ve ever felt bloated, foggy, or just “off” after eating, your gut may be trying to tell you something. The term “leaky gut” is more than a wellness buzzword — it’s a growing area of research connecting digestive health to everything from mood and energy to inflammation and immunity. Your gut isn’t just where food is digested; it’s also where your immune system, hormones, and even neurotransmitters are finely tuned. When this system gets out of balance, your entire body feels the effects.
What Is Leaky Gut?
Your intestines are designed to act as a smart filter — allowing nutrients, water, and electrolytes to pass through while blocking toxins and waste. The inner lining of your gut is made up of a single layer of specialized cells called enterocytes. These cells are held together by tight junctions, microscopic gates that open and close selectively. Under normal circumstances, it’s an elegantly efficient system that keeps you healthy and nourished.
But modern life can overwhelm this barrier. Processed foods, chronic stress, medications, and toxins can cause those tight junctions to loosen. When this happens, unwanted substances — bits of undigested food, bacteria, and endotoxins — slip through the gaps and enter the bloodstream. Your immune system immediately reacts as if it’s under attack. This chain reaction is what scientists refer to as increased intestinal permeability, or what’s commonly known as leaky gut.
Once that inflammatory switch is flipped, it can stay “on” indefinitely, showing up in unexpected ways: fatigue, headaches, rashes, low mood, or even joint pain. In other words, your gut’s health is tied to nearly every system in your body.
Common Causes of Leaky Gut
While genetics can make some people more vulnerable, lifestyle factors are the biggest contributors. Here’s what often sets the stage for trouble:
- Poor diet: Highly processed foods, excess sugar, refined carbs, and seed oils damage the gut lining and disrupt the microbiome.
- Chronic stress: Elevated cortisol weakens digestive function and slows repair of the gut wall.
- Sleep deprivation: Sleep is when your body regenerates tissues, including your intestinal lining.
- Medications: Frequent use of antibiotics, NSAIDs, or acid blockers can alter gut flora and irritate the lining.
- Alcohol and smoking: Both increase oxidative stress and inflammation, accelerating barrier breakdown.
- Nutrient deficiencies: Zinc, vitamin D, omega-3s, and antioxidants are crucial for maintaining tight junctions.
- Microbiome imbalance: Too many harmful bacteria and not enough beneficial ones create a perfect storm for permeability.
Even environmental toxins — from pesticides to heavy metals — can chip away at your gut’s defenses over time. The modern world makes it nearly impossible to avoid all of these triggers, which is why proactive support is so valuable.
Symptoms You Might Notice
Because your gut communicates with nearly every system in your body, symptoms of leaky gut can seem unrelated. You might visit multiple specialists before realizing they’re all connected to the same root cause. Here are some of the most common red flags:
- Persistent bloating, gas, or abdominal discomfort
- Irregular bowel movements (constipation or loose stools)
- Food sensitivities or intolerance to foods you once enjoyed
- Brain fog, trouble concentrating, or fatigue after meals
- Skin issues such as acne, eczema, or rosacea
- Joint stiffness or muscle aches without clear injury
- Mood changes, anxiety, or irritability due to gut-brain imbalance
Left unchecked, this low-grade inflammation can set the stage for autoimmune conditions, metabolic dysfunction, and accelerated aging. That’s why addressing gut integrity early can make such a dramatic difference in how you feel day to day.
Healing a Leaky Gut Naturally
The good news is that your gut lining renews itself roughly every five to seven days. With the right nutrition and lifestyle habits, you can begin the repair process quickly. Here’s a practical roadmap:
- Eat clean, whole foods: Focus on vegetables, lean proteins, and healthy fats. Bone broth, garlic, and onions contain natural prebiotics that feed beneficial bacteria.
- Cut down on sugar and alcohol: Both promote growth of harmful bacteria and increase inflammation.
- Support your microbiome: Add fermented foods like yogurt, kefir, kimchi, or sauerkraut, or take a well-formulated probiotic.
- Manage stress: Chronic stress alters gut motility and secretions. Daily mindfulness, light walking, or deep breathing can calm the gut-brain axis.
- Get adequate sleep: Aim for 7–8 hours to allow for cellular regeneration, including the intestinal lining.
- Supplement strategically: L-glutamine supports mucosal repair; zinc carnosine strengthens tight junctions; and Tributyrin provides targeted fuel for the cells that rebuild your gut barrier.
Consistency is key — think of gut healing as a restoration project, not an overnight fix. Each meal and habit either contributes to healing or adds to the damage, so small daily choices add up.
Spotlight: Tributyrin by BodyHealth — The Gut Healer
One of the most advanced tools for gut restoration is Tributyrin, a highly absorbable form of butyrate — a short-chain fatty acid your gut microbes naturally produce when you eat fiber. Butyrate is like fuel for your colon cells; without enough of it, those cells weaken and the gut barrier starts to fail. Tributyrin delivers butyrate deeper into the intestines, where it can do the most good.
🔥 Seals & Heals the Gut Lining
- Stimulates regeneration of the protective mucous layer
- Repairs “tight junctions,” sealing microscopic leaks
- Helps your gut cells generate energy for faster recovery
🧘♀️ Supports Natural Inflammatory Processes
- Encourages a balanced immune response rather than overreaction
- Regulates gene expression linked to cellular repair and detoxification
🌿 Supports Microbiome Balance
- Feeds beneficial bacteria that crowd out harmful strains
- Promotes production of calming neurotransmitters such as GABA and serotonin, explaining why a healthy gut often means a better mood
💪 Promotes Resilient Digestion & Energy
- Reduces occasional bloating and discomfort after meals
- Improves nutrient absorption, so the food you eat actually nourishes you
- Supports steady energy by reducing inflammation-related fatigue
In today’s world of fast food, chronic stress, and environmental toxins, Tributyrin can help restore the foundation of health — your gut lining. It’s also part of BodyHealth’s Gut Support Protocol, a comprehensive system designed to address every layer of gut repair. You can take Tributyrin on its own or combine it with complementary nutrients for even greater results.
💊 Ready to start healing your gut?
Click here to discover Tributyrin by BodyHealth — and start strengthening your gut from the inside out.
Beyond Digestion: The Gut-Brain Connection
Your gut and brain are in constant conversation through what scientists call the gut-brain axis. Signals travel along the vagus nerve and through chemical messengers like serotonin and dopamine — nearly 90% of which are produced in the gut. When your gut is inflamed or imbalanced, it can send “distress” signals that affect mood, focus, and motivation. That’s why improving gut health often leads to clearer thinking and greater emotional stability.
Butyrate, the active component in Tributyrin, plays a key role here as well. It nourishes the gut lining, supports the microbiome, and reduces neuroinflammation — helping you feel not just better physically, but mentally sharper and calmer too.
The Takeaway
Your gut health influences everything — digestion, energy, mood, immunity, and even longevity. By understanding and addressing leaky gut, you give your body the foundation it needs to thrive. Focus on nourishing foods, restorative sleep, stress balance, and targeted supplements like Tributyrin. Over time, you’ll notice smoother digestion, brighter energy, clearer skin, and a lighter mood — all signs your gut barrier is healing.
As an affiliate, I may earn a small commission if you purchase through my link — at no additional cost to you.
Explore Gut Support Supplements on Fullscript |
Harvard Health: The Link Between Gut Health and Overall Wellness
by Dr. Richard J. Walicki | Oct 19, 2025 | Dentistry, Hacks
Banana peel whitening hack videos seem to be everywhere—but this one might actually damage your teeth. Let’s look at what really happens when you mix banana peel, lemon, salt, and toothpaste together.
The banana peel whitening hack is one of those viral “natural” tricks that looks clever in a short video—until you understand what’s really happening to your enamel. The recipe is simple: scrape the inside of a banana peel, mix in a little lemon juice, salt, and toothpaste, then brush. The post I saw even promised you’ll “get results without paying for your dentist’s yacht.”
As a dentist—and for the record, a completely yacht-free one—I felt compelled to step in. Let’s explore what this banana peel teeth whitening hack actually does, why it’s risky, and what science-backed methods will give you a brighter, healthier smile instead.
Why This Banana Peel Hack Seems to Work
At first glance, the banana peel whitening hack sounds almost logical. Bananas contain minerals like potassium and magnesium. Lemons have natural acids that “clean.” Salt is a traditional scrubber, and toothpaste is already in everyone’s bathroom. Mix them all together and you might think you’ve invented the ultimate natural whitener. Unfortunately, chemistry disagrees.
Lemon juice is extremely acidic—around pH 2 to 3, similar to vinegar or soda. Enamel starts dissolving at a pH below 5.5. That means the lemon juice doesn’t just lift stains; it actually begins dissolving the mineral structure of your teeth. Once enamel softens, even gentle brushing causes surface loss. Add salt and toothpaste—both mildly abrasive—and you’re effectively sanding your enamel smooth.
So yes, the banana peel whitening hack can make teeth look slightly brighter, but that’s because it’s removing micro-layers of enamel. It’s not true whitening; it’s acid etching. Light reflects differently off a roughened surface, giving the illusion of brightness—much like buffing metal until it shines.
 What the Banana Peel Really Does
What the Banana Peel Really Does
Supporters of the banana peel to whiten teeth trend claim that minerals from the peel soak into enamel to rebuild it. Enamel, however, is not porous tissue—it’s a crystalline shield. Minerals can’t simply “absorb” through contact with fruit pulp. Remineralization happens internally through saliva, and enamel hardens with fluoride, not through banana peels.
At best, rubbing with a banana peel might dislodge surface debris. At worst, combined with lemon acid and salt, it contributes to irreversible wear. The peel itself isn’t harmful, but the mixture amplifies damage.
Short-Term Results, Long-Term Damage
One use of the banana peel teeth whitening hack probably won’t destroy your smile, but repeating it regularly creates serious risks:
- Enamel erosion: Once the outer layer thins, the underlying yellow dentin shows through, making teeth look darker over time.
- Sensitivity: Worn enamel exposes tiny tubules that carry sensations directly to the nerve.
- Staining: Roughened enamel traps pigments from coffee, tea, or red wine more easily. Over time, this hack could actually set you up for darker teeth.
- Gum irritation: Acids and abrasives inflame soft tissue, leading to tenderness or peeling along the gumline.
People often interpret these symptoms as “detoxing” or “deep cleaning.” In truth, they’re signs of chemical abrasion—the loss of the very substance that keeps your teeth strong and insulates them from harm.
The Science of Safe Whitening
Real whitening happens when controlled peroxide compounds break down colored molecules within enamel without destroying its mineral matrix. That’s how professional whitening and ADA-approved products work. According to the American Dental Association (ADA), peroxide treatments—used in safe concentrations—change tooth color chemically, not mechanically.
In dental offices, gels with hydrogen or carbamide peroxide gently penetrate enamel pores to dissolve stains, leaving the structure intact. At home, whitening strips or peroxide toothpastes achieve gradual brightening safely, though usually somewhat less effectively. The big difference between those and the banana peel whitening hack is testing: professional products are proven effective; social-media mixtures are not.

Natural Ways to Keep Teeth Bright
If you prefer natural maintenance, there are safer approaches than experimenting with acidic fruit. Try these instead of any DIY banana peel whitening hacks:
- Brush twice daily with a non-abrasive toothpaste and soft bristles—no heavy scrubbing needed.
- Floss daily to remove plaque that dulls enamel and causes gum inflammation.
- Rinse with water after coffee, tea, or citrus to neutralize acids and reduce staining, or drink water afterward to rebalance pH.
- Eat crunchy produce like apples or carrots. They gently polish teeth and increase saliva flow.
- Get professional cleanings twice a year for stain removal that preserves enamel.
These habits may sound less exciting than a viral video, but they protect enamel and deliver lasting brightness.
Why Dentists Speak Out (and Most Still Don’t Own Yachts)
The viral post insists you can whiten your teeth “without paying for your dentist’s yacht.” Funny line—but misleading. Dentists don’t get rich off whitening visits. We earn trust by helping patients keep their natural teeth for life. When we warn against the banana peel whitening hack, it isn’t because we want to sell you something; it’s because we’ve seen enamel loss up close. The damage from acid and abrasion is permanent.
Personally, I’d rather have patients who keep their enamel intact than ones who need fillings and sensitivity treatments later. So if I ever did buy a yacht, it would be named The Enamel—and I’d still be reminding people not to dissolve theirs.
The Real Takeaway
Before mixing fruit and toothpaste, remember that the banana peel whitening hack offers only illusion, not improvement. It may promise a “natural” shortcut, but natural doesn’t always mean safe. Real whitening involves science, patience, and protecting what nature already gave you. Your enamel is a non-renewable resource—once it’s gone, it’s gone for good.
For more myth-busting articles like this one, explore our
Tooth Truth or Myth? series on social media or check out our Weird Dental Facts page..
You’ll find practical insights on dental fads, oral-health tips, and proven ways to keep your smile strong for years to come.
by Dr. Richard J. Walicki | Oct 14, 2025 | Dentistry, Periodontal Disease
Introduction: Gum Disease and Brain Health
Definition of Gum Disease
Gum disease (periodontal disease) is a chronic inflammatory condition driven by bacterial biofilms. It often begins as
gingivitis (gum inflammation and bleeding) and can progress to periodontitis, where the attachment between gum and tooth breaks down. In periodontitis, pathogenic biofilm extends subgingivally, pockets deepen, and supporting bone may be lost. Untreated disease increases the risk of tooth loss and is associated with systemic effects beyond the oral cavity, including potential effects on brain health.
Overview of Brain Health
Brain health encompasses the integrity of cognitive functions—memory, attention, processing speed, and executive function—supported by strong vascular and metabolic systems. Factors such as age, sleep, physical activity, nutrition, and oral health all contribute to maintaining long-term cognitive resilience.
Why Explore the Connection?
The connection between gum disease and brain health has gained attention as evidence accumulates that oral pathogens and chronic periodontal inflammation may influence neuroinflammatory pathways. Oral bacteria and their by-products can enter the bloodstream, potentially reach the central nervous system, and contribute to
brain inflammation. While Alzheimer’s disease and other dementias are multifactorial, periodontal status appears to be a modifiable risk factor.
Key Insight: Periodontal disease is associated with higher cerebrovascular risk; several studies report an increased likelihood of stroke in individuals with moderate to severe periodontitis.
Understanding the link between gum disease and brain health supports practical strategies for prevention. Evidence-based periodontal care—plaque control, smoking cessation, and professional therapy—may reduce inflammatory burden relevant to cognitive wellness.
The Science Behind Gum Disease
Causes of Gum Disease
Periodontitis is initiated by dysbiotic bacterial communities within dental plaque. Contributing factors include inadequate oral hygiene, tobacco use, systemic disease, hormonal fluctuations, and genetic predisposition. These factors combine to amplify inflammation and tissue destruction, elevating overall risk to brain health.
- Poor oral hygiene: inadequate plaque removal and infrequent dental care.
- Smoking: suppresses immune response and delays healing.
- Hormonal changes: puberty, pregnancy, and menopause may heighten gingival sensitivity.
- Systemic conditions: diabetes and metabolic disorders exacerbate inflammation.
- Genetics: individual variations in immune response influence disease susceptibility.
Stages of Gum Disease
The disease advances through stages with increasing tissue breakdown and greater systemic impact, potentially influencing brain health.
| Stage |
Description |
Symptoms |
| Gingivitis |
Reversible inflammation confined to gingiva. |
Bleeding, redness, mild swelling. |
| Mild Periodontitis |
Early attachment loss, shallow pockets. |
Halitosis, minor mobility, calculus buildup. |
| Moderate Periodontitis |
Progressive loss of bone and tissue support. |
Deeper pockets, recession, discomfort. |
| Severe Periodontitis |
Extensive tissue destruction, potential tooth loss. |
Mobility, bleeding, pain, and visible bone loss. |
Without treatment, periodontal inflammation increases the body’s systemic load, which may influence gum disease and brain health outcomes.
Symptoms and Diagnosis
Early periodontal changes can be silent. Common symptoms include:
- Bleeding gums: during brushing or flossing.
- Persistent bad breath: from anaerobic bacterial activity.
- Receding gums: exposing sensitive root surfaces.
Dentists diagnose periodontal disease by measuring pocket depths and evaluating radiographic bone levels. Early detection not only preserves teeth but may also reduce inflammation affecting gum disease and brain health.
Takeaway: Routine periodontal evaluations and maintenance therapy lower local inflammation and can reduce systemic inflammatory exposure linked to cognitive decline.
The Impact of Gum Disease on Overall Health
Systemic Effects of Untreated Gum Disease
In the context of gum disease and brain health, untreated periodontitis contributes to persistent bacteremia and immune activation. Pathogens and inflammatory mediators may travel to distant organs, including the brain, where they can contribute to neuroinflammation and tissue damage.
Links to Other Chronic Conditions
- Diabetes: inflammation worsens glycemic control, and high glucose impairs immune response.
- Cardiovascular disease: inflammation contributes to atherosclerosis and endothelial dysfunction.
- Respiratory disease: aspiration of oral bacteria may aggravate chronic lung conditions.
Key Insight: Chronic inflammation is a shared pathway between gum disease, cardiovascular health, and cognitive decline.
Understanding Brain Health
Factors That Influence Brain Health
- Nutrition: diets rich in omega-3s, antioxidants, and vitamins support cognition.
- Exercise: improves blood flow and promotes neuroplasticity.
- Sleep: allows cellular repair and toxin clearance.
- Stress management: reduces cortisol-driven inflammation.
- Oral health: lowers systemic inflammatory exposure, indirectly protecting the brain.
The Oral-Systemic Connection
Oral health and brain health are linked through inflammation and vascular pathways. Periodontal pathogens have been detected in brain tissue, suggesting a plausible biological route between gum disease and brain health.
Takeaway: Prioritizing oral care through professional cleanings, good home hygiene, and healthy lifestyle choices supports both oral and cognitive wellness.
Research and Evidence
Numerous studies have explored the relationship between gum disease and brain health. For example, researchers have identified periodontal pathogens such as Porphyromonas gingivalis in the brains of patients with Alzheimer’s disease. Chronic periodontal inflammation may contribute to systemic cytokine release, vascular changes, and neuroinflammatory responses—all associated with cognitive decline.
Key Insight: While gum disease does not directly cause dementia, reducing oral inflammation through professional treatment may lower systemic risk factors influencing cognitive aging.
Prevention and Management
Home Care Practices
- Brush twice daily with a soft-bristled or powered toothbrush.
- Clean interdentally once per day with floss or interdental brushes.
- Rinse with an antimicrobial mouthwash as advised by your dentist.
- Maintain professional cleaning visits every 3–4 months as needed.
Nutrition and Lifestyle
- Limit sugar intake: to minimize bacterial growth.
- Consume anti-inflammatory foods: such as leafy greens, berries, and fatty fish.
- Stay hydrated: saliva supports natural cleansing and remineralization.
Cognitive Support Tip: A healthy mouth reduces inflammatory load, which benefits both cardiovascular and neurological health.
Prevention remains the cornerstone for maintaining gum disease and brain health together. Regular professional care, home hygiene, and lifestyle optimization protect both your smile and your mind.
Further reading on ToothWiz:
How dental infections spread beyond a tooth ·
Supplements that promote gum and immune health ·
Nutrients that support brain and gut function
References:
American Academy of Periodontology – periodontal bacteria linked to Alzheimer’s ·
Meta-analysis: Oral bacteria and cognitive decline ·
Forsyth Institute – Gingival bacteria and amyloid plaque
This article is for educational purposes only and is not a substitute for professional dental or medical advice. Patients should consult their dentist or physician for personalized recommendations.
by Dr. Richard J. Walicki | Oct 4, 2025 | Dentistry
Introduction
Welcome to the ultimate showdown: tooth abscess vs cyst.
It may not be the latest Marvel release, but the plot twists in your mouth can be just as dramatic.
If you’ve felt a sharp twinge when you bite, spotted a puffy spot on the gum, or noticed a slow-growing bump on an X-ray,
you may be wondering whether you’re dealing with a true infection-driven abscess or a
dental cyst.
Spoiler: they’re not the same thing—yet they can look similar from the outside.
In this post, I’ll break down what each condition is, why it happens, how it’s diagnosed, and what treatment usually looks like.
Think Batman vs. Superman: both powerful but with different missions. The same goes for abscesses and cysts—both occupy space, both can threaten surrounding structures,
but their causes and ideal treatment paths diverge in important ways.
Quick primer: A dental abscess is a pocket of pus caused by infection.
A cyst is a fluid-filled sac that can form in bone or soft tissue.
One is primarily about bacteria; the other is about pathologic tissue growth.
Telling them apart matters because the treatment differs.
Abscesses often announce themselves with pain, swelling, and tenderness—sometimes fever.
Cysts, on the other hand, can be stealthy for a long time.
They may quietly expand, thinning bone or nudging teeth until they’re big enough to be noticed on a routine X-ray.
Both can be serious if ignored.

Understanding Tooth Abscesses
What a Tooth Abscess Is (and Isn’t)
A tooth abscess is an infection that your body walls off as a pocket of pus.
Bacteria invade the pulp (the living core of the tooth) through deep decay, a crack, or trauma.
When pulp tissue dies or becomes infected, pressure builds and inflammation ramps up.
The infection seeks a path of least resistance—often through the root tip or along the gum.
Dental vs. Periodontal Abscess—Important Clarification:
A periapical (dental) abscess starts inside the tooth and exits near the root tip after bacteria reach the pulp.
A periodontal abscess starts in the gum and supporting bone around a tooth—usually from deep periodontal pockets or trapped debris.
Treatment focuses on the source: root canal therapy for a periapical abscess; periodontal therapy (and sometimes surgery) for a periodontal abscess.
Common Causes
- Untreated cavities: Deep decay opens a highway for bacteria to reach the pulp.
- Cracks or fractures: Even hairline cracks can allow bacteria in.
- Trauma: A blow to a tooth may damage pulp tissue and set the stage for infection.
- Failed or incomplete prior treatment: If bacteria persist after a procedure, infection can re-emerge.
- Advanced gum disease: Deep pockets can become walled-off infection sites.
Symptoms You Might Notice
- Throbbing pain that can radiate to the jaw, ear, or temple; often worse with chewing or heat.
- Swelling in the gum or face; sometimes a visible “pimple” (fistula) on the gum that drains.
- Tenderness to bite or pressure; the tooth may feel “taller” than neighbors.
- Pus drainage and a bad taste or odor.
- Fever / malaise in moderate to advanced infections.
How Dentists Diagnose Abscesses
- Percussion and palpation: Tapping and pressing help gauge inflammation.
- Pulp vitality testing: Cold tests assess nerve response.
- Periodontal probing: Looks for deep pockets or isolated defects suggesting a periodontal abscess.
- X-rays / CBCT: Reveal radiolucency, widened ligament space, or bone loss patterns.
Why the source matters:
A periapical abscess calls for root canal therapy; a periodontal abscess calls for periodontal debridement and drainage.
Treating one when you actually have the other can delay healing.
Treatment Options
- Drainage: Opening the tooth or gum pocket to release pressure and pus.
- Root canal therapy: Cleans and seals the canal system when infection originates inside the tooth.
- Periodontal therapy: Debridement, irrigation, and sometimes surgery for gum-based abscesses.
- Extraction: When the tooth cannot be saved.
- Antibiotics: Used only when systemic signs like fever or swelling are present—never as the sole fix.

Left untreated, abscesses can spread to adjacent spaces and threaten overall health.
If pain or swelling escalates—or you develop fever—see your dentist promptly.
Understanding Dental Cysts
What a Dental Cyst Is
A dental cyst is a pathologic, fluid-filled sac lined by epithelium that forms in the jaws or soft tissue.
Some cysts are tied to tooth development (odontogenic); others arise after chronic irritation or from remnants of dental tissues.
Unchecked expansion can thin bone, shift teeth, or encroach on nerves or sinuses.
Common Types
- Radicular cysts: Associated with non-vital teeth after long-standing infection.
- Dentigerous cysts: Form around unerupted teeth, often wisdom teeth or canines.
- Eruption cysts: Seen in children; usually self-limiting.
- Odontogenic keratocysts: Notorious for recurrence, requiring careful follow-up.
Why Cysts Form
- Post-infection stimulation: Chronic inflammation can trigger cyst formation.
- Developmental factors: Disturbances in tooth development may leave remnants that form cysts.
- Impacted teeth: Pressure and follicular fluid buildup contribute to dentigerous cysts.
- Genetic or syndromic conditions: Certain disorders predispose patients to multiple cysts.
Symptoms
- Often painless until large.
- Jaw swelling or fullness.
- Shifting or loosening teeth.
- Numbness if nerves are compressed.
- Pain or drainage if secondarily infected.
Note: Even painless cysts can weaken bone and shift teeth. Most require removal or careful monitoring.
Diagnosis and Treatment
- X-rays / CBCT: Define size, location, and relationship to teeth or sinuses.
- Vitality testing: Distinguishes cysts tied to dead teeth from other lesions.
- Biopsy or aspiration: Confirms diagnosis and rules out other pathology.
Treatment typically means removal: Most cysts are surgically excised (enucleation) or decompressed before removal.
Follow-up imaging ensures full healing and detects recurrence.

Abscess vs Cyst: The Key Differences
The right diagnosis is crucial because treatment options differ significantly between these two conditions.
Ignoring proper diagnosis is like trying to guess what’s in a mystery box—you might end up with something you didn’t expect!
| Feature |
Tooth Abscess |
Dental Cyst |
| Cause |
Bacterial infection of pulp or gum |
Pathologic fluid-filled sac |
| Pain |
Common, often throbbing |
Minimal until large |
| Onset |
Acute or acute-on-chronic |
Slow, progressive |
| Exam clues |
Tenderness, swelling, pus |
Expansion, tooth shift |
| Imaging |
Periapical radiolucency |
Well-defined radiolucency |
| Primary treatment |
Drainage + root canal / periodontal therapy |
Surgical removal or decompression |
Bottom line: Abscesses are infections that need source control.
Cysts are lesions that need removal or decompression.
They can look similar on the surface—exam and imaging are essential.
When to See a Dentist
Red Flags
- Severe or escalating pain
- Swelling in face or gums
- Pus discharge or foul taste
- Fever or malaise
- Difficulty swallowing or breathing
- Numbness or shifting teeth
A timely diagnosis can mean the difference between simple treatment and extensive surgery.
Don’t wait until a minor issue becomes a major one.
Prevention: Lowering Your Risk
Practical Habits
- Brush twice daily with gentle technique.
- Floss or use interdental cleaners every day.
- Rinse with antimicrobial mouthwash if prone to inflammation.
- Limit sugary snacks and drinks.
- Stay hydrated to maintain saliva flow.
- Avoid smoking or chewing tobacco.
Dental Visits
- Catch silent problems early with X-rays.
- Spot periodontal pockets before infection sets in.
- Professional cleanings reduce hidden bacterial load.
- Personalized prevention plans prevent escalation.
A study in the Journal of Dental Research found that patients with routine visits had significantly fewer abscesses than those who delayed care.
Regular check-ups pay off.
FAQs
Can a cyst turn into an abscess?
A cyst can become secondarily infected and act like an abscess, but the processes differ.
Both the infection and the cyst itself need to be addressed.
Do abscesses always need antibiotics?
Not always. The cornerstone is source control—drainage and, if periapical, root canal therapy.
Antibiotics are for systemic signs such as fever or spreading cellulitis.
What if my tooth doesn’t hurt but an X-ray shows a dark area?
That could be a chronic periapical lesion or cyst.
Your dentist will test the tooth, review imaging, and decide whether endodontic treatment or surgical removal is best.
Can home care fix an abscess?
No. Salt-water rinses may soothe tissues, but an abscess requires professional intervention.
Conclusion
Abscesses and cysts can look alike but behave very differently.
Abscesses signal infection that needs elimination; cysts signal a lesion that needs removal or monitoring.
Recognizing the difference—and acting early—protects your comfort, your teeth, and your jaw.
Remember: Small dental problems don’t age well.
If something feels off—pain, swelling, a gum bump, or an odd X-ray—get it evaluated.
You’ll save time, money, and stress by treating the real cause sooner rather than later.
For more quirky-but-useful reading, visit the
Weird Dental Facts section.
For wellness support that complements oral health, explore
ToothWiz Vitamins.
Additional Resources and References
Your dentist is your best ally in diagnosing tooth abscess or cyst issues.
Regular check-ups can help catch these problems early!

by Dr. Richard J. Walicki | Sep 28, 2025 | Dentistry
Introduction to Perfect Amino
What is Perfect Amino?
Perfect Amino is a premium essential amino acid supplement created by BodyHealth. Unlike many traditional protein powders, which may be incomplete or difficult to digest, Perfect Amino delivers a precise amino acid profile designed for maximum efficiency. Nearly all of it is absorbed and used by the body for protein synthesis, tissue repair, and recovery—making it a clean, highly effective protein alternative.
 Why amino acids are essential
Why amino acids are essential
Amino acids are the building blocks of protein. Out of the 20 amino acids, nine are considered essential—meaning the body cannot make them, and they must come from diet or supplementation. These essential amino acids (EAAs) play key roles in:
- Repair and Recovery: Supporting the rebuilding of muscle and connective tissue.
- Strength and Mass: Helping to preserve or grow lean muscle.
- Energy: Acting as a secondary energy source during activity.
- Immunity & Hormones: Contributing to defense and regulation systems.
This is where Perfect Amino shines: it delivers a complete, balanced supply of EAAs in an easily absorbed form, ensuring your body has what it needs to thrive.
Amino acids aren’t just about building muscle—they’re critical for immune defense, metabolic health, and hormone regulation. (Source: Harvard T.H. Chan School of Public Health)
Comparing protein sources
Protein is available from meat, dairy, plants, and supplements—but each has limitations. Here’s a side-by-side view:
| Protein Source |
Pros |
Cons |
| Animal Proteins (meat, dairy) |
– Complete amino profile
– High in BCAAs
– Efficient absorption |
– Often high in saturated fats
– Ethical & environmental concerns |
| Plant Proteins (legumes, grains) |
– Lower in calories
– High in fiber
– Vegan-friendly |
– May lack certain EAAs
– Require combining for completeness |
| Powdered Proteins (whey, soy) |
– Convenient
– Fortified
– Fast absorbing |
– May cause bloating
– Allergens (lactose, soy) |
The advantage of Perfect Amino? It offers a complete essential amino acid spectrum without the calories, fillers, or digestive discomfort of many traditional sources.
Takeaway:
The right protein source impacts performance, recovery, and long-term health. Perfect Amino provides an efficient, well-balanced option that helps bridge gaps in traditional diets.
The Science Behind Perfect Amino
Formulation and efficiency
Perfect Amino contains all nine essential amino acids in ratios optimized for human health. Unlike most proteins, where 30–50% may go unused, Perfect Amino achieves a net nitrogen utilization (NNU) of over 90%—meaning almost everything you consume contributes to protein metabolism and repair.
Why it outperforms food proteins
- Absorption speed: Utilized within 30 minutes—much faster than meat or dairy.
- Completeness: Covers all nine EAAs without food combining.
- Tolerability: Free from gluten, lactose, and common allergens.
Bioavailability
Efficiency matters: whey protein is absorbed at ~50–70%, casein lower, while Perfect Amino exceeds 90%. This superior absorption means faster recovery and better results with less waste.
Studies show that essential amino acid blends like Perfect Amino support muscle recovery significantly more than whey alone. (Source: Journal of the International Society of Sports Nutrition)
Perfect Amino and Dental Health
As a dentist, I’ve seen firsthand how nutrition impacts oral health. Amino acids—especially lysine, proline, and threonine—are central to collagen production, which forms the foundation of gum tissue, ligaments, and bone structure. Without enough amino acids, gum repair and post-treatment healing slow dramatically.
- Stronger Gums: Supports collagen in gum tissue, reducing susceptibility to periodontal breakdown.
- Faster Healing: Aids recovery after extractions, implants, or surgery.
- Tissue Integrity: Helps maintain the protein framework that stabilizes dentin and enamel minerals.
For patients struggling with gum disease, tissue healing, or recovery from dental work, Perfect Amino can be a valuable addition to their overall care plan.
Dental Insight:
Nutrition is the foundation of oral health. Supplementing with Perfect Amino helps reinforce gum resilience, healing, and the long-term stability of your smile.
Nutritional and Lifestyle Benefits
Muscle recovery and performance
By fueling protein synthesis, Perfect Amino helps speed recovery, reduce soreness, and support lean muscle gains more effectively than incomplete proteins or BCAAs alone.
Energy, mood, and cognition
EAAs are precursors to neurotransmitters like serotonin and dopamine, supporting focus, balanced mood, and steady energy. They also reduce protein breakdown, helping sustain energy throughout the day.
Wellness beyond athletics
Perfect Amino contributes to hormone regulation, immune resilience, and healthy aging—making it useful for athletes and non-athletes alike. Combined with BiOptimizers supplements, it can be part of a broader strategy for performance and longevity.
Conclusion: Making Protein Work for You
Perfect Amino is more than a fitness supplement. It’s an efficient, complete, and well-tolerated protein source that supports muscle recovery, steady energy, and even dental health. Whether you’re an athlete pushing performance or simply aiming for better overall wellness, it can be a smart addition to your nutritional strategy.
✅ Ready to Experience the Difference?
This essential amino acid formula by BodyHealth is designed to maximize absorption, fuel recovery, and even support oral health.
👉 Order Now from BodyHealth
Want more supplement options? Visit ToothWiz Vitamins.
Your Takeaway:
Perfect Amino delivers high-value nutrition in a simple form. From faster recovery to stronger gums, it provides the building blocks your body—and your smile—depend on.For more on supporting your health with supplements, explore ToothWiz Vitamins or check out my Top Picks from BiOptimizers.
by Dr. Richard J. Walicki | Sep 20, 2025 | Dentistry
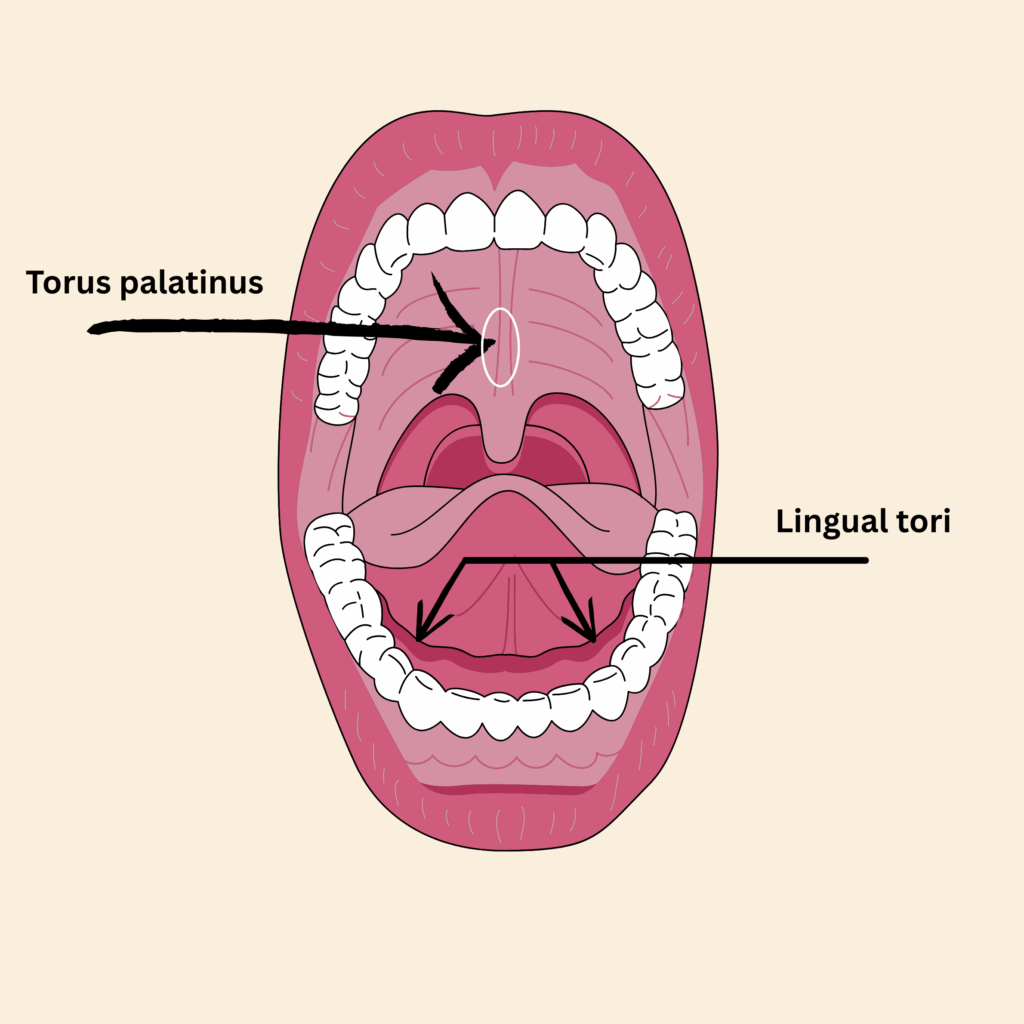
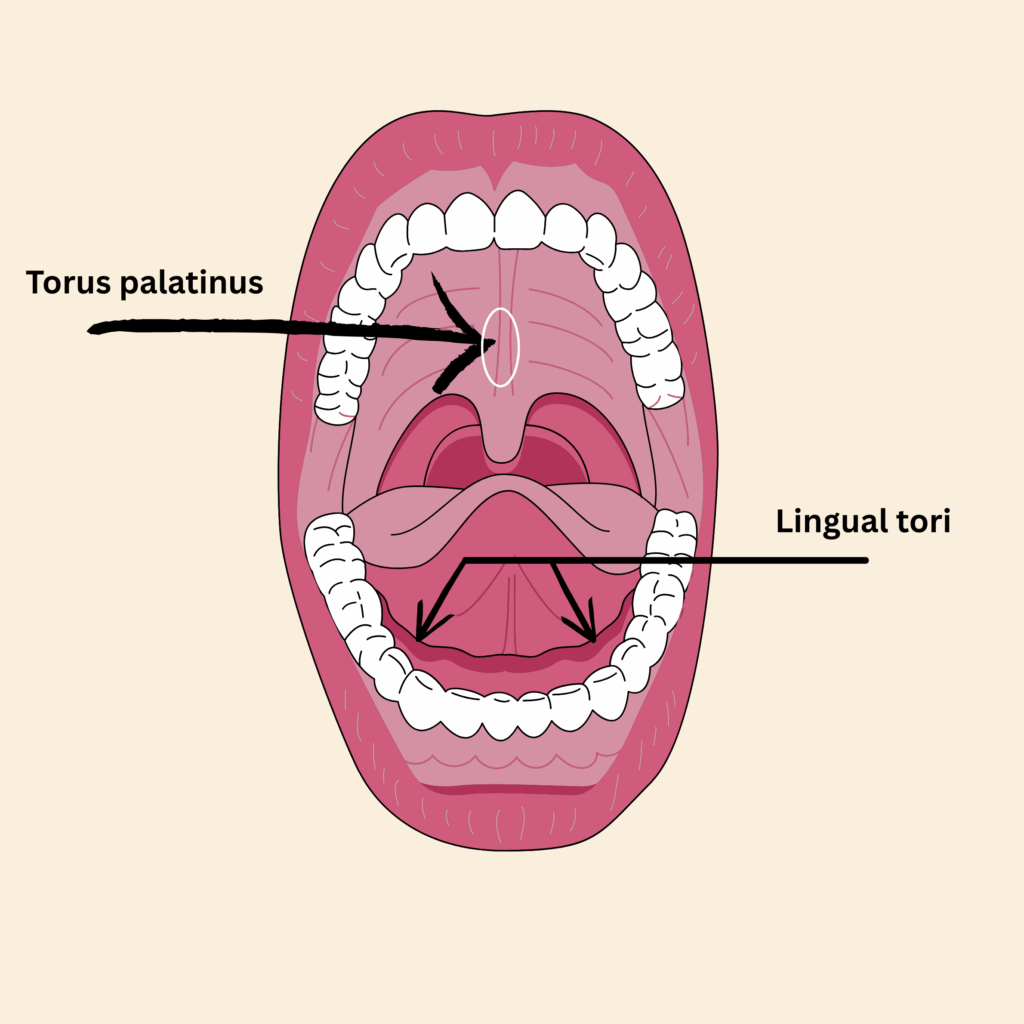
So, what exactly are oral exostoses? In simple terms, it refers to bony growths in the mouth, also known as oral tori. A single bony growth is called an exostosis. When more than one occurs, they are referred to as exostoses. These benign oral growths can appear on various parts of the mouth, including the hard palate and along the jawbone. Think of them as your body’s way of saying, “Hey, I’ve got some extra bone here!” The most common types include:
- Torus palatinus: A bony protrusion on the roof of the mouth.
- Torus mandibularis: Growths that occur along the lower jaw.
- Buccal exostosis: Bumps on the inside of the cheeks.
- Gingival exostosis: Growths on the gums.
- Alveolar ridge exostosis: Bony growths along the tooth-bearing areas.
These growths are typically non-cancerous and may not cause any symptoms at all, making them quite sneaky!
In fact, most patients are unaware they even have tori or buccal exostoses until a dentist points them out. They rarely cause problems on their own, but their presence can become a major concern when dentures are needed. Large mandibular tori in particular may make it difficult — or even impossible — to comfortably wear a lower denture. In such cases, removal may be necessary before prosthetic treatment can proceed.
Treatment options usually involve surgical removal with a bur and chisel or more modern laser-assisted removal. Traditional surgery tends to involve more postoperative swelling and a longer healing period, while laser procedures may reduce bleeding and shorten recovery time. Your dentist or oral surgeon can help determine which option is appropriate based on the size, location, and complexity of the bony growths.
Importance of recognizing symptoms
Recognizing symptoms associated with oral exostosis is crucial. While many people might have these bony protrusions in their mouth cavity, they often go unnoticed until they cause discomfort or complications. Ignoring symptoms could lead to issues like:
- Pain or discomfort when chewing or speaking.
- Difficulties with bite alignment.
- Persistent swelling in the gums or jaw area.
- The appearance of hard lumps in the mouth that could be mistaken for something more serious.
If left unchecked, these benign bone growths can become a nuisance. So, keeping an eye out for changes in your oral health is essential!
Overview of the blog post structure
This blog post will dive into the top 5 symptoms of oral exostosis you shouldn’t ignore. We will cover:
- Pain or discomfort in the jaw – what it feels like and when to seek help.
- Swelling in the gums or jaw area – how to differentiate normal from concerning swelling.
- Changes in bite alignment – how these bony growths can affect your dental health long-term.
- The presence of hard bumps in your mouth – physical symptoms to monitor over time.
This comprehensive guide aims to equip you with knowledge about oral exostosis, ensuring you recognize any potential red flags early on. Knowledge is power when it comes to your dental health!
Your smile deserves attention! Stay informed about changes in your oral health, and don’t hesitate to consult a professional if something feels off. Remember: proactive care beats reactive treatment any day!
Symptom 1: Pain or Discomfort in the Jaw
Explanation of pain types associated with oral exostoses
If you’ve ever felt a nagging discomfort in your jaw, it might not just be a sign of stress from your daily grind. Pain or discomfort in the jaw can be one of the first symptoms of exostosis oral. This pain can manifest in various ways, and understanding what you’re feeling is key to addressing it.
- Localized pain: This is when you feel discomfort right where the bony growths are located, like a gentle reminder that something’s up.
- Dull ache: You might experience a persistent ache that seems to radiate throughout your jaw, making you wonder if your jawbone has taken up an interest in heavy lifting.
- Shooting pain: Sometimes, you might feel sharp pangs that catch you off guard, especially when chewing or speaking. It’s like your mouth just decided to throw a surprise party – and not the fun kind!
- Tenderness: The area around the bony protrusions may feel tender to touch. You might find yourself avoiding certain foods just to keep things comfortable.
This discomfort could stem from pressure exerted by the bony growths in your mouth, which can lead to inflammation or irritation of surrounding tissues. In some cases, it may even affect your bite alignment, creating a ripple effect on how you chew and speak.
When to seek professional help
If you’re experiencing any type of jaw pain, it’s essential not to ignore it. Here are some signs that indicate it’s time to consult a dental professional:
- Your discomfort persists for more than a few days – no one wants an unwelcome guest hanging around!
- The pain intensifies over time or starts affecting your daily activities like eating or talking.
- You notice swelling or changes in the appearance of your gums near the painful area – this could indicate possible complications.
- If you have difficulty opening or closing your mouth comfortably – it’s best to get checked out before things escalate.
Pain is often an indicator that something needs attention. Don’t brush off those signals! Early intervention can lead to more effective treatment options for oral exostosis, reducing potential complications down the line.
Symptom 2: Swelling in the Gums or Jaw Area
Causes of swelling related to exostosis oral
Swelling in the gums or jaw area can be one of the more noticeable symptoms of exostosis oral. But what causes this swelling? Well, think of it as your body’s way of throwing a little tantrum! Here are some common culprits:
- Pressure from bony growths: As bony protrusions in the mouth cavity grow, they can create pressure on surrounding tissues, leading to inflammation and swelling.
- Irritation: If food particles or plaque get trapped around these growths, it can cause irritation and subsequent swelling. It’s like having a party in your mouth that nobody wanted to be invited to!
- Infection: In some cases, a localized infection can occur, resulting in significant swelling. This is your body’s way of saying, “Help! I need a dentist!”
- Gingivitis: Inflammation of the gums due to poor oral hygiene can exacerbate swelling around exostosis areas. So, brushing and flossing are essential-consider them your mouth’s bodyguards!
If you notice any unusual swelling, it’s crucial to pay attention. It could be a sign that something more serious is brewing beneath the surface.
Differentiating between normal and concerning swelling
Not all swelling is created equal! Knowing when to chill and when to seek help is vital. Here’s how you can differentiate between normal and concerning swelling:
- Normal Swelling: A slight puffiness around the gum line or jaw area that comes and goes might just be an indication of irritation from food or brushing too hard.
- Concerning Swelling: If you experience persistent or increasing swelling that lasts more than a few days, it’s time to consult a professional. This could indicate an underlying issue related to oral exostosis.
- Pain Accompaniment: Normal swelling might not hurt much; however, if there’s pain associated with the swelling-especially if it intensifies-don’t ignore it!
- Changes in Gum Color: Healthy gums should be pink; if they appear red, swollen, or bleeding along with the swelling, this could signal gingivitis or another issue.
Your mouth is talking! Pay attention to what it’s saying. Swelling might seem minor at first but can escalate into more serious problems like infections if left unchecked. Regular check-ups with your dentist are key!

Matthew Ferguson 57, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons
Symptom 3: Changes in Bite Alignment
Description of how exostosis can affect bite
Imagine your mouth as a finely tuned orchestra, where each tooth plays its part in harmony. Now, throw in some oral exostoses and suddenly, that symphony turns into a cacophony! Changes in bite alignment are a common symptom of oral exostosis, and they can be quite the nuisance.
As those bony growths in the mouth develop-be it torus palatinus or torus mandibularis-they can interfere with how your teeth come together. Here’s how:
- Pressure Points: When these bony protrusions push against teeth, they can create uneven pressure, leading to a misaligned bite. Think of it as one musician playing too loudly and throwing off the entire performance.
- Shifting Teeth: Over time, the displacement caused by these growths may result in teeth shifting positions. It’s like trying to fit a square peg into a round hole-something’s gotta give!
- Tenderness and Discomfort: The discomfort from misalignment can lead to further issues like jaw pain or headaches. Your body might start sending out distress signals, reminding you that something is amiss.
If you notice your bite feels different or if you’re experiencing discomfort while chewing, it might be time to investigate whether oral exostosis is at play.
Potential long-term impacts on dental health
Inevitably, ignoring changes in bite alignment due to dental exostosis can lead to some serious long-term consequences. Here’s what could happen if you let those pesky bony growths take center stage:
- Cavities and Tooth Decay: Misaligned bites can make certain areas harder to clean, increasing the risk of cavities. If your toothbrush can’t reach those nooks and crannies, plaque will throw a party-and not the fun kind!
- TMD (Temporomandibular Disorder): A misaligned bite can stress your jaw joints over time, leading to TMD. This could result in jaw pain, clicking sounds when opening your mouth, or even migraines. Ouch!
- Dental Anomalies: The longer you wait to address bite issues caused by oral tori, the more likely you are to develop other dental anomalies that may require extensive treatment.
- Aesthetic Concerns: A misaligned bite may affect your smile’s aesthetics too! If you’re self-conscious about how your teeth line up, it could impact your confidence-and we all know how important a radiant smile is!
Your dental health is interconnected! Changes in bite alignment due to exostosis oral are not just about comfort; they can have lasting effects on overall oral health. Don’t hesitate-consult with a professional if you notice any changes!
Symptom 4: Difficulty Chewing or Speaking
How oral exostosis can interfere with daily activities
Picture this: you’re at a dinner party, and everyone is laughing and enjoying their food. But you? You’re over here struggling to chew your delicious meal because of exostosis oral. It’s like trying to run a marathon in flip-flops-definitely not ideal! Difficulty chewing or speaking can be a significant symptom of oral exostosis, and it can really put a damper on your social life.
As those pesky bony growths in the mouth develop, they can create discomfort that makes even the simplest tasks like biting into a sandwich feel like an Olympic event. Here’s how this might play out:
- Chewing Challenges: When bony protrusions, such as torus mandibularis or torus palatinus, push against your teeth or cheeks, it can lead to pain while chewing. It’s as if your mouth is saying, “Thanks, but no thanks!” to that juicy burger.
- Sore Spots: The friction between these growths and the inside of your mouth can create sore spots that make speaking feel like an endurance test. You might find yourself avoiding certain words just to keep from wincing!
- Mouth Movement Restrictions: If the growths are large enough, they may restrict how wide you can open your mouth. Imagine trying to sing your favorite song but only being able to whisper the lyrics-frustrating, right?
If you notice these difficulties creeping into your daily life, it’s time to take note! Ignoring them could lead to more significant issues down the line.
Signs that indicate a need for evaluation by a dentist
If you’ve been experiencing difficulty chewing or speaking due to oral exostosis, there are some telltale signs that should prompt you to seek professional help:
- Persistent Pain: If the discomfort lasts longer than a few days or worsens over time-don’t wait for it to go away on its own!
- Avoidance Behavior: If you find yourself avoiding certain foods or conversations because of pain-this is not just an inconvenience; it’s a signal from your body!
- Mouth Opening Issues: Difficulty opening your mouth wide enough for normal activities like yawning or eating could indicate that those bony growths need attention.
- Speech Changes: If friends start asking why you’re mumbling or slurring words, it might be time for a dental check-up!
Your ability to chew and speak comfortably is essential for enjoying life! Don’t hesitate to reach out to a dental professional if you’re facing challenges related to exostosis oral. Early intervention could save you from more complex treatments later!

Symptom 5: Presence of Hard Bumps in the Mouth
Description of physical symptoms to look for
So, you’ve noticed some hard bumps in your mouth? Well, it’s time to pay attention! These hard lumps could be a sign of oral exostosis, and while they might not cause immediate alarm, they can lead to more serious issues if left unchecked. Here are some characteristics to look for:
- Location: These bony growths can appear on various parts of the mouth, including the hard palate (think torus palatinus) or along the jawline (hello, torus mandibularis). They might even pop up on the inside of your cheeks as buccal exostoses.
- Texture: Feel free to poke around (gently!). If you notice that these bumps feel firm and hard rather than soft or swollen, you’re likely dealing with benign oral growths.
- Size: While some bumps may remain small and asymptomatic, others can grow larger over time. If they start feeling like they’re auditioning for a role in a monster movie, it’s definitely time to consult your dentist!
- Pain or Discomfort: Although many cases are asymptomatic, if these growths start causing discomfort or pain while eating or speaking, that’s your cue to take action.
If you’re unsure about what you’re feeling in your mouth, don’t hesitate to reach out to a dental professional. They can help determine whether those pesky bumps are just harmless bone growths or something that requires further investigation.
Importance of monitoring changes in oral health over time
Your mouth is a window into your overall health! Monitoring changes related to an oral exostosis, such as the presence of hard lumps in your mouth, is crucial for maintaining good oral hygiene. Here’s why keeping an eye on these changes matters:
- Early Detection: Noticing changes early can help catch potential complications before they escalate. Think of it as being proactive rather than reactive-your future self will thank you!
- Avoiding Misdiagnosis: Hard bumps can sometimes resemble other conditions that may require different treatments. By staying vigilant and reporting any changes to your dentist, you reduce the risk of misdiagnosis.
- Treatment Options: If those bony protrusions start causing problems, there are various treatment options available-from monitoring the growths through regular check-ups to considering oral surgery for exostosis. The earlier you address them, the more options you’ll have!
- Mouth Health Matters: Keeping track of any new developments in your oral cavity helps ensure that you’re maintaining optimal oral health. After all, a healthy smile is a happy smile!
Your mouth is like a garden-regular maintenance keeps it flourishing! Make sure to monitor any changes and consult with your dentist about any concerns regarding oral exostosis. Your smile deserves it!
Your Call to Action
As we wrap up this exploration of oral exostoses, it’s clear that recognizing the symptoms is crucial for maintaining your oral health. We’ve covered:
- Pain or discomfort in the jaw
- Swelling in the gums or jaw area
- Changes in bite alignment
- Difficulty chewing or speaking
- Presence of hard bumps in the mouth
The significance of these symptoms cannot be overstated. Ignoring them could lead to complications that are easily avoidable with early intervention.
Your dental health is interconnected with your overall well-being! If you’re experiencing any of these symptoms, don’t hesitate to reach out to a dental professional. Early detection and treatment options for an oral exostosis, including dental torus removal, can save you from more extensive procedures down the line.
According to a 2012 Case Reports in Dentistry paper, Er:YAG lasers have been successfully used to excise mandibular tori and smooth torus palatinus exostoses, offering good clinical healing though sometimes requiring more operative time than conventional burs. PMC
Clinical review sources also support laser removal as less traumatic with reduced post-operative pain, swelling, and bleeding. Dentistry Today+1
Current Understanding of Causes and Symptom Relief
The exact cause of oral tori is not fully understood. However, studies suggest they are influenced by a combination of genetic and environmental factors. Environmental contributors include parafunctional habits such as bruxism (tooth grinding) and clenching, as well as occlusal stress. Research also indicates a higher prevalence of mandibular tori in patients with TMD (temporomandibular disorders) or excessive bite force. Thus, the bony over-growth may be a reaction to the excessive forces placed on the teeth and underlying bone. Sort of nature’s way of “bulking up” against stress.
Because these bony growths develop slowly and progressively, there is currently no proven way to prevent them. Instead, most home measures focus on symptom relief and reducing irritation:
- Warm saltwater rinses: Can reduce irritation and soothe tissues around the growths.
- Aloe vera gel: Offers mild anti-inflammatory relief when applied to irritated areas.
- Good oral hygiene: Helps reduce local irritation from plaque or trapped food near tori.
- Soft food choices: Avoiding very hard or abrasive foods may minimize trauma to areas where exostoses protrude.
Your mouth is an ecosystem! While you can’t prevent an oral exostosis from forming, supportive care can reduce discomfort. Remember: their development is linked to genetics and bite forces more than daily hygiene habits.

by Dr. Richard J. Walicki | Sep 18, 2025 | Dentistry
Introduction to Yaeba
Ah, yaeba. This quirky dental trend has taken the world by storm, particularly among young adults in Japan. But what is yaeba exactly? In short, it refers to the deliberate alteration of one’s teeth to create a charmingly imperfect smile. Think of it as the dental equivalent of wearing your favorite vintage band tee—deliberately worn but undeniably cool.
Definition of Yaeba
At its core, yaeba teeth are characterized by their crookedness, particularly the canine teeth that protrude slightly. This aesthetic is not just a random fad; it’s a carefully curated look that embodies a unique blend of beauty and individuality. The yaeba smile has become synonymous with youthfulness and playfulness—traits highly valued in modern Japanese culture.
Origin of the Trend
The roots of this trend can be traced back to traditional Japanese beauty norms that have long celebrated imperfection as a form of charm. The concept aligns well with the idea of charming crooked teeth, which many find endearing. It’s almost like how we adore our favorite quirky characters in movies—flaws make them relatable and lovable!
The yaeba trend surged in popularity around 2008, largely influenced by celebrities flaunting their own yaeba smiles. These celebrity endorsements sparked a wave of interest among fans eager to replicate that unique look. A survey conducted by the Japanese Association of Orthodontists found that 41% of respondents preferred women with yaeba, highlighting its cultural significance.
Significance in Japanese Culture
The yaeba trend reflects deeper cultural beauty standards in Japan, where uniqueness is often celebrated over conventional perfection. While traditional aesthetics prized straight and white teeth, modern sensibilities have shifted towards embracing individuality through trends like yaeba cosmetic dentistry.
This shift represents a broader acceptance of diverse beauty standards in Japan and beyond. As young adults increasingly seek out ways to express their identity through their appearance, yaeba serves as a striking example of how personal expression can manifest even in something as fundamental as our smiles.
Interestingly, this trend isn’t limited to Japan; it has sparked interest globally as people explore various dental fashion statements. From tooth reshaping Japan techniques to the rising popularity of braces designed specifically for achieving that coveted yaeba look, it’s clear that this trend is here to stay.

The Appeal of Yaeba Among Young Adults
Psychological Factors Influencing Attraction to Imperfections
The allure of yaeba among young adults can be partly attributed to psychological factors. In a world dominated by polished perfection, there’s something refreshingly rebellious about embracing flaws. This trend taps into a deep-rooted desire for authenticity and individuality. Think of it as the beauty equivalent of a well-loved, slightly worn-out book; it tells a story and feels relatable.
Research shows that people are often drawn to imperfections because they evoke warmth and approachability. A study in the Journal of Experimental Social Psychology found that people perceive those with minor flaws as more likable and trustworthy. So, when young adults choose a yaeba smile, they are not just altering their appearance; they are making a statement about who they are.
Social Media’s Role in Popularizing Yaeba
If you’ve ever scrolled through Instagram or TikTok, you know how quickly trends can catch fire. The yaeba trend is no exception! Social media platforms have played a significant role in popularizing this unique dental fashion statement. With influencers showcasing their own yaeba smiles, the trend has spread like wildfire, encouraging others to embrace their own quirks.
- Influencer Impact: Many young adults follow influencers who flaunt their yaeba teeth, leading to increased interest in the dental procedure.
- Visual Appeal: The striking visuals of yaeba smiles make them highly shareable, creating a ripple effect across social media platforms.
- Cultural Exchange: As the trend gains traction outside Japan, it fosters a cultural exchange that highlights different beauty standards globally.
This digital exposure has made yaeba more than just a passing fad; it’s become part of an ongoing conversation about beauty norms and self-expression.
Cultural Shifts Towards Embracing Uniqueness and Individuality
The rise of yaeba reflects broader cultural shifts towards embracing uniqueness and individuality—not just in Japan but around the globe. As traditional beauty standards evolve, many young adults are seeking ways to express their identity through their appearance. This is particularly true in countries where conventional aesthetics have long dominated.
A 2011 survey by Oricon Style ranked yaeba as one of the top beauty trends in Japan, illustrating its growing acceptance among youth and its impact on cultural beauty standards.
This shift is not merely cosmetic; it represents a deeper desire for self-acceptance and personal expression. Young adults today are more inclined to celebrate what makes them different rather than conforming to outdated ideals of perfection. The yaeba dental procedure, whether achieved through traditional braces or modern techniques like tooth reshaping, allows individuals to embrace their unique smile aesthetics while challenging societal norms.
 If you’re intrigued by the idea of adopting your own version of this charming crooked teeth beauty trend, remember: it’s all about celebrating your individuality! Whether you’re considering yaeba braces or simply want to explore unique smile aesthetics, take inspiration from those who have already embraced this playful approach to dental fashion.
If you’re intrigued by the idea of adopting your own version of this charming crooked teeth beauty trend, remember: it’s all about celebrating your individuality! Whether you’re considering yaeba braces or simply want to explore unique smile aesthetics, take inspiration from those who have already embraced this playful approach to dental fashion.
Yaeba and Dental Health: A Holistic Perspective
Understanding the Impact of Yaeba on Oral Health
While the yaeba trend is undeniably charming, it raises important questions about dental health. The deliberate alteration of teeth to achieve that coveted yaeba smile can have implications beyond aesthetics. For instance, crooked teeth beauty may enhance one’s appearance, but they can also lead to issues like misalignment and difficulty in cleaning.
Many young adults considering this trend should be aware of the potential for increased plaque buildup or even gum disease due to hard-to-reach areas created by double tooth trends. Regular dental check-ups become even more critical for those sporting a yaeba look, ensuring that their unique smiles remain healthy.
Comparative Analysis with Traditional Dental Aesthetics
The traditional view of dental aesthetics emphasizes straight, white teeth as the gold standard. However, the emergence of yaeba challenges this notion. While traditional braces focus on achieving uniformity, yaeba braces often aim for a more playful and imperfect look.
| Aspect |
Traditional Aesthetics |
Yaeba Aesthetics |
|
| Appearance Goal |
Straight and uniform teeth |
Crooked and charmingly imperfect smile |
|
| Treatment Focus |
Crowding correction and alignment |
Cultivating uniqueness through selective alteration |
|
| Cultural Perception |
Perfection is idealized |
Imperfection is celebrated as authentic beauty |
|
| Dental Procedure Type |
Braces and aligners for straightening teeth |
Yaeba dental procedure: cosmetic alterations to create desired imperfections |
|
The Importance of Preventive Care in Maintaining Dental Wellness Despite Cosmetic Choices
If you’re thinking about jumping on the yaeba bandwagon, remember that preventive care is your best friend! Regular brushing, flossing, and dentist visits are essential to keep your unique smile healthy. Here are some tips for maintaining oral wellness while indulging in aesthetic choices:
- Stay Consistent: Brush at least twice a day and don’t forget to floss! This helps minimize plaque buildup around those charmingly crooked areas.
- Mouthwash Matters: Using an antibacterial mouthwash can help reduce bacteria in hard-to-reach spots.
- Dentist Check-Ups: Schedule regular check-ups every six months to catch any potential issues early on.
- Nutritional Choices: Eating a balanced diet rich in calcium can support overall dental health while you flaunt your unique style!
- Avoid Hard Foods: Be cautious with hard candies or nuts that could damage your altered teeth.
- Sensitivity Awareness: If you experience sensitivity due to tooth modifications, consult with your dentist about protective options.
- Mental Health Check: Embrace your unique smile but also be aware of how societal pressures might affect your self-esteem; remember that beauty comes in many forms!
The key takeaway? You can rock a fabulous
yaeba smile, but don’t forget about keeping those pearly whites healthy! After all, a radiant smile starts with good care.
The Process of Achieving Yaeba: What You Need to Know
Cosmetic Procedures Available for Enhancing Yaeba
If you’re ready to embrace the yaeba trend, there are several cosmetic procedures that can help you achieve that charmingly imperfect smile. Here’s a quick rundown:
- Yaeba Braces: Unlike traditional braces that aim for straightness, yaeba braces are designed to enhance the crookedness of your teeth. They focus on creating a playful, youthful appearance.
- Veneers: These thin shells can be applied to your teeth to create the desired look of imperfections without altering the actual structure of your teeth.
- Bonding: Dental bonding allows for selective reshaping of certain teeth, giving them that coveted yaeba aesthetic while maintaining overall dental health.
- Tooth Reshaping: This involves minor alterations to the shape and size of your teeth to enhance their unique characteristics, fitting perfectly within the double tooth trend.
While these procedures can help you achieve a distinctive yaeba smile, it’s essential to consult with a qualified dentist who understands this unique aesthetic. They can guide you through the best options tailored to your individual needs.
Natural Methods to Achieve a Similar Look Without Invasive Procedures
If you’re not quite ready for cosmetic alterations but still want to channel that natural yaeba look, there are some non-invasive methods you can explore:
- Mouth Exercises: Certain mouth exercises can help create subtle shifts in your smile. Think of it as yoga for your jaw!
- Lip Positioning: Playing with how you position your lips while smiling can give off a more relaxed, imperfect vibe—perfect for channeling yaeba without any changes!
- Dental Wax: Some individuals use dental wax temporarily on their teeth to mimic imperfections while they figure out their next steps.
- Cultural Embrace: Simply embracing and showcasing your natural smile with confidence can often reflect the essence of yaeba without any modifications.
Considerations and Potential Risks Associated with Altering Dental Aesthetics
Before pursuing a yaeba smile, it’s crucial to consider potential risks and implications for your oral health. Here are some key points to keep in mind:
- Dental Health Risks: Altering your teeth might lead to complications like misalignment or difficulty cleaning, which could increase plaque buildup and gum disease risk.
- Cultural Rebellion vs. Personal Choice: While embracing yaeba may feel like a rebellion against Western beauty ideals, ensure that the choice resonates personally.
- Candidacy Concerns: Not everyone is an ideal candidate for yaeba procedures—existing dental health should be evaluated by a professional first.
- Pain and Discomfort: Some procedures may involve discomfort during treatment or recovery.
- Misinformation Awareness: Always seek expert advice over anecdotal experiences from social media influencers.
The bottom line? While achieving a stunning
yaeba smile may seem exciting, it’s essential to think about aesthetics and long-term oral health.
The Future of Yaeba: Trends and Predictions
Potential Evolution of the Trend in Different Cultures
The yaeba trend isn’t just a fleeting moment in Japan; it’s poised to evolve and adapt across cultures. As global beauty standards shift, we may see a rise in similar trends that celebrate imperfections in dental aesthetics.
The Role of Influencers and Celebrities in Shaping Perceptions of Beauty Standards
Influencers and celebrities have propelled the yaeba trend globally, normalizing this once-niche aesthetic and encouraging a wider conversation about beauty norms.
Predicting the Sustainability of Yaeba as a Long-Term Trend Among Young Adults
Sustainability depends on cultural relevance, evolution, and dental health awareness. Experts caution that altering teeth for aesthetics can lead to long-term dental issues (Japan Today).
Wrapping Up: Embracing Individuality in Dental Health Choices
The Importance of Informed Decision-Making Regarding Dental Aesthetics
As we close out our deep dive into the yaeba trend, it’s essential to highlight the importance of making informed choices. Whether you’re considering a yaeba dental procedure or simply contemplating your smile’s aesthetic, understanding the implications is key.
A Holistic Approach to Oral Health and Beauty Standards
Yaeba reflects cultural shifts towards individuality and rejecting conventional beauty standards. In Japan, cultural beauty standards have long celebrated imperfections. Globally, the trend is also gaining traction.
Encouragement for Readers to Embrace Their Unique Smiles While Prioritizing Wellness
Celebrate what makes you unique while prioritizing your oral health. Whether you choose yaeba braces, explore non-invasive options, or embrace your natural smile, authenticity is key.