The Affordable Dentist
Let’s face it: seeing a doctor – any sort of doctor – can be expensive. And dentists are no exception. But if a person’s diet and home care have been lacking, the cost of dental treatment can quickly sky-rocket. One of the problems with dental care has to do with the fact that many patients still suffer from the idea that if they don’t feel anything wrong with their teeth, then all is well.
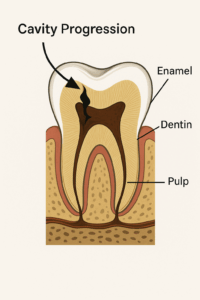
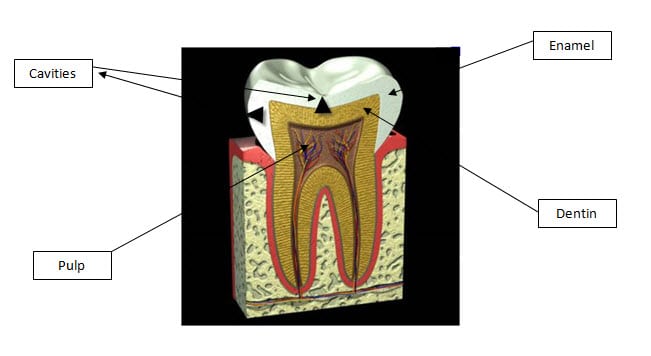
Unfortunately, when it comes to teeth, most people miss the boat entirely with this concept. The reason is simple: the outer part of the tooth – the enamel – is mostly mineral and has no nerves. That means you can have a cavity and not know it. Several, actually. Most dentists will attest to the fact that many patients are shocked to learn they have any cavities at all.
The trouble is that by the time a cavity actually gets big enough to pose a problem, it’s a PROBLEM. For most people that trouble is spelled P-A-I-N.
It’s really no small wonder that so many individuals associate going to the dentist with toothaches. For those patients, it is the only time they will actually make an appointment. They go because they now know they have a cavity. Pain is a huge motivator. . . .
By the time a tooth hurts, though, the cavity is usually pretty close to the nerve. This means that if there is still enough tooth structure left to work with, the dentist may consider a root canal to remove the source of the pain – in other words – the nerve. Usually, this is not cheap. A root canal on a molar can cost over a thousand dollars when performed by a specialist. Then the patient has to go back to the dentist to have the tooth built up again (because so much tooth structure was lost to decay) and finally, the tooth may even need a crown. Lacking a blood supply and nerve thanks to the root canal, the tooth is now brittle and can break. Since your back teeth get a lot of pressure when you chew, failing to crown it may result in the tooth cracking and all that money you spent on the root canal goes out the window.
In a number of cases, because many people simply fear getting a root canal (not because they actually had one, but because they heard that a friend of a friend had a bad experience, and they never want to go through THAT), they opt to remove the tooth instead.
But now they have to replace the missing tooth or else their teeth will shift around and their bite goes awry. And fixing that new problem typically costs even more!
It can be frustrating.
Many people figure no one will see a missing back tooth, so why not pull it, since that is cheaper? At least they think so – until they notice their front teeth starting to form gaps, and find that food gets stuck all over the place whenever they eat. But then again, what if it’s a front tooth that needs to go?
You possibly think: “Wow, this is a problem, but I still really need to find something cheap.” OK, then. If you live in Philadelphia, you may Google “affordable Philadelphia dentist” or “cheap dentist.” A number of listings for dental implants appear, maybe some for “affordable cosmetic dentistry.” Wow, this isn’t sounding at all affordable!!! Wait! A couple of dental schools come up too. “Hmmm. Do I really want someone in their first year of dental clinic restoring my front tooth? It will be less expensive. But, then again . . . .”

In the meantime, it is essential to keep yourself out of trouble with good preventive dental practices. Learn what diet has to do with your teeth and which home care habits are best. Remember, when it comes to teeth and gums, “no pain” most definitely does not always mean “no problems”.