You CAN Take Care of Your Teeth
The idea that losing teeth is an inevitable part of aging is a common misconception. While it’s true that tooth loss occurs more frequently among older adults, it’s not a foregone conclusion. With proper oral care and preventive measures, you can keep your natural teeth healthy and strong well into your later years.
Why Tooth Loss Occurs
Tooth loss can be caused by various factors, including:
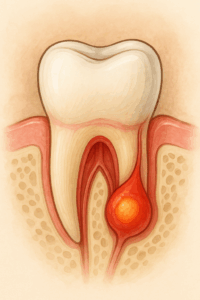
- Gum disease: This is the leading cause of tooth loss in adults. Gum disease is an infection that affects the soft tissues around the teeth, eventually destroying the bone that supports them.
- Tooth decay: This is caused by bacteria that build up on the teeth and form plaque. Plaque produces acids that can erode the enamel, the hard outer covering of the teeth. If left untreated, tooth decay can lead to cavities and eventually tooth loss.
- Trauma: Injuries to the mouth or teeth can also cause tooth loss.
- Other health conditions: Certain medical conditions, such as osteoporosis and diabetes, can increase the risk of tooth loss.
Preventive Measures
The good news is that you can take steps to prevent tooth loss and maintain healthy teeth for a lifetime. Here are some key strategies:
- Practice good oral hygiene: This includes brushing your teeth twice a day for two minutes each time, flossing daily, and using a mouthwash.
- Visit your dentist regularly: For professional cleanings and checkups.
- Eat a healthy diet: Limit sugary foods and drinks, which can contribute to tooth decay.
- Quit smoking: Smoking increases the risk of gum disease and other oral health problems.
In addition to these general recommendations, there are some specific things you can do to protect your teeth as you age:
- Use a toothbrush with soft bristles: Hard bristles can damage your gums and enamel.
- Consider using an electric toothbrush: Electric toothbrushes can be more effective at removing plaque and bacteria than manual toothbrushes.
- Get regular fluoride treatments: Fluoride can help strengthen your teeth and prevent decay.
Myths about Tooth Loss and Aging
There are several common myths about tooth loss and aging. Here are a few of the most prevalent:
- Myth: Losing teeth is a natural part of aging.
- Fact: While tooth loss is more common among older adults, it’s not inevitable. With proper oral care, you can keep your teeth healthy for a lifetime.
- Myth: You don’t need to see the dentist as often as you get older.
- Fact: It’s important to continue seeing your dentist regularly for checkups and cleanings, even as you get older. Regular dental care can help detect and prevent problems early on.
- Myth: There’s nothing you can do to prevent tooth loss.
- Fact: There are many things you can do to prevent tooth loss, including practicing good oral hygiene, eating a healthy diet, and quitting smoking.
Losing teeth doesn’t have to be a part of aging. With proper care and preventive measures, you can enjoy a healthy smile for a lifetime. Talk to your dentist about ways to keep your teeth healthy and strong as you age.
Additional Resources
- The American Dental Association: https://www.ada.org/
- The National Institute of Dental and Craniofacial Research: https://www.nidcr.nih.gov/
- The Oral Health Foundation: https://www.dentalhealth.org/